Welcome to the captivating world of laryngoscopy and anesthesia! Laryngoscopy is a medical procedure that involves using an instrument to look inside the throat and larynx. This procedure is used to diagnose and treat various conditions such as vocal cord paralysis, airway obstruction, and infection. Anesthesiologists are essential for laryngoscopy, as they administer the necessary medications and monitor the patient’s vital signs during the procedure. In this blog, we will explore the different types of laryngoscopy, the benefits of laryngoscopy, the role of anesthesia during this procedure, and the potential complications associated with laryngoscopy. We will also discuss the importance of proper preparation and choosing the right anesthesiologist for the procedure. So, let’s take a peek into the amazing world of laryngoscopy and anesthesia!
What is laryngoscopy?
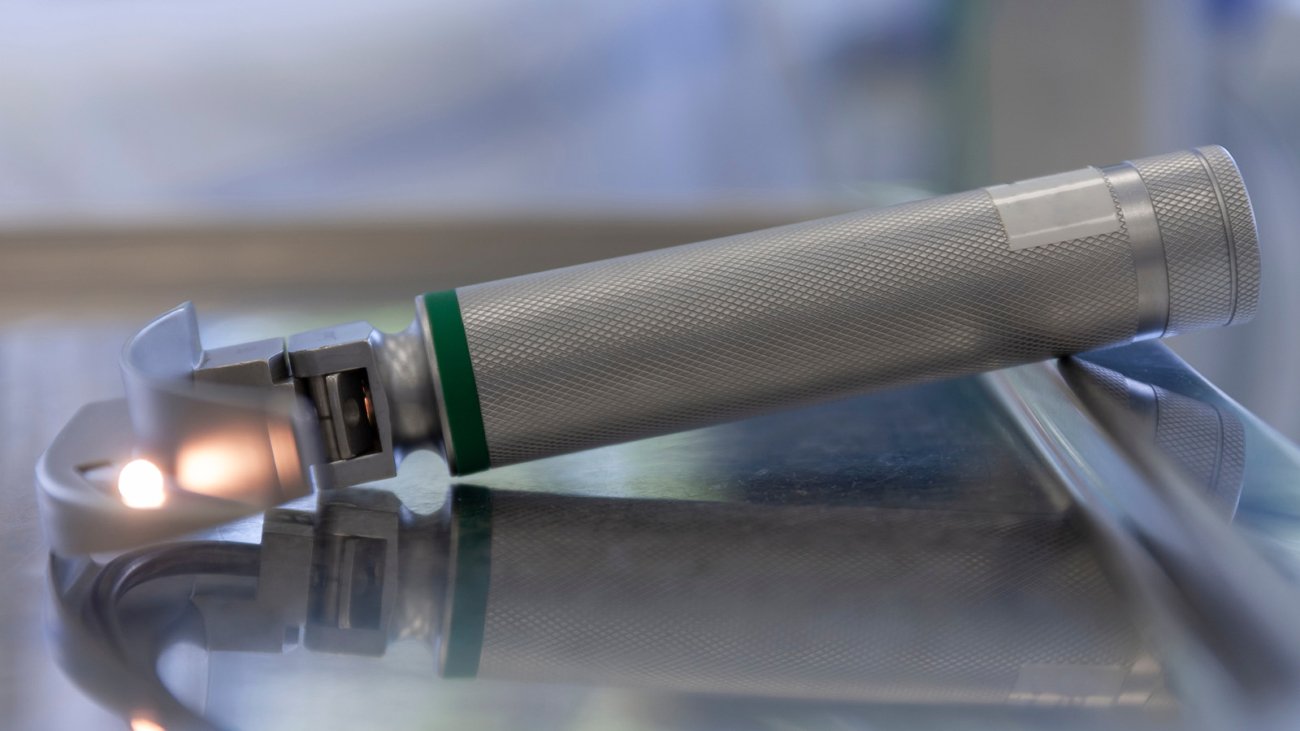
Laryngoscopy is a medical procedure that involves the use of an instrument called a laryngoscope to look inside the throat and larynx. The procedure is used to diagnose and treat various conditions such as vocal cord paralysis, airway obstruction, and infection. During the procedure, the laryngoscope is inserted through the mouth or nose and then into the throat and larynx. This allows the doctor to view the larynx and look for any abnormalities. If any issues are found, they can then be addressed. The procedure is performed under local anesthesia, which numbs the area where the laryngoscope is inserted.
Types of laryngoscopy
There are several different types of laryngoscopy. The most common type is direct laryngoscopy, which involves inserting a rigid laryngoscope into the throat and larynx. The doctor can then use the laryngoscope to inspect the area and take biopsies, if needed. Other types of laryngoscopy include indirect laryngoscopy, fiber-optic laryngoscopy, and virtual laryngoscopy. Indirect laryngoscopy uses a flexible laryngoscope to inspect the larynx. Fiber-optic laryngoscopy uses a fiber-optic scope to view the larynx, while virtual laryngoscopy uses high-resolution images to view the larynx.
Benefits of laryngoscopy
Laryngoscopy is a very beneficial procedure. It can help diagnose and treat a variety of conditions. It can also be used to evaluate the voice, detect laryngeal cancer, or detect other structural or functional abnormalities. The procedure can also be used to treat vocal cord paralysis, airway obstruction, and infection. In addition, laryngoscopy can be used to assess the effects of anesthetic agents, to evaluate the response to drugs, and to detect any adverse reactions to medications.
Anesthesia and the use of laryngoscopy
Anesthesia is essential for laryngoscopy. Anesthesiologists are responsible for administering the necessary medications and monitoring the patient’s vital signs during the procedure. During laryngoscopy, anesthesiologists will typically use a combination of local, regional, and general anesthetics to ensure the patient is comfortable and safe during the procedure. Local anesthetics are used to numb the area where the laryngoscope is inserted. Regional anesthetics are used to provide additional pain relief and relaxation. General anesthetics are used to induce unconsciousness and put the patient in a deep sleep.
Potential complications of laryngoscopy
Although laryngoscopy is generally safe, there are some potential risks and complications associated with the procedure. These include bleeding, infection, and damage to the vocal cords. In rare cases, the procedure can cause serious complications such as airway obstruction, aspiration, and respiratory depression. It is important to discuss any potential risks and complications with your doctor prior to the procedure.
Preparing for a laryngoscopy
It is important to prepare for a laryngoscopy to ensure the procedure goes smoothly. Before the procedure, your doctor will likely provide you with instructions on how to prepare. These may include avoiding eating or drinking for a certain amount of time prior to the procedure, avoiding certain medications, and avoiding strenuous activity. Your doctor may also ask you to wear a hospital gown and provide detailed information about your medical history.
How to choose an anesthesiologist
Choosing the right anesthesiologist is essential for laryngoscopy. Anesthesiologists are responsible for administering the necessary medications and monitoring the patient’s vital signs during the procedure. It is important to find an experienced anesthesiologist who is knowledgeable about the procedure and the medications being used. It is also important to ensure the anesthesiologist is licensed and certified in the state where the procedure is being performed.
Guidelines for anesthesia during laryngoscopy
There are certain guidelines that anesthesiologists must follow during laryngoscopy. These guidelines include monitoring the patient’s vital signs, monitoring the effects of medications, and avoiding the use of certain medications. It is also important to ensure that the patient is properly positioned during the procedure to avoid any potential complications. Additionally, the anesthesiologist must be aware of any allergies or underlying medical conditions the patient may have so that the necessary precautions can be taken.
Risks associated with laryngoscopy and anesthesia
Although laryngoscopy and anesthesia are generally safe, there are some risks associated with the procedures. These risks include bleeding, infection, airway obstruction, aspiration, and respiratory depression. Additionally, there is a risk of an allergic reaction to the medications used during the procedure. It is important to discuss these risks with your doctor prior to the procedure.
Conclusion
We hope this blog has given you an insight into the amazing world of laryngoscopy and anesthesia. Laryngoscopy is a medical procedure that involves using an instrument to look inside the throat and larynx. Anesthesiologists are essential for laryngoscopy, as they administer the necessary medications and monitor the patient’s vital signs during the procedure. There are various types of laryngoscopy and many benefits associated with the procedure. However, it is important to understand the potential risks and complications associated with laryngoscopy and anesthesia. It is also important to ensure proper preparation and to choose the right anesthesiologist for the procedure.
If you are considering laryngoscopy and anesthesia, it is important to speak to your doctor about the risks and benefits of the procedure. Your doctor can help you make an informed decision and provide you with the necessary information to ensure the procedure is safe and successful.
Laryngoscopy and anesthesia can be a beneficial and safe procedure when performed correctly. We hope this blog has given you an insight into the amazing world of laryngoscopy and anesthesia and the potential risks and benefits associated with the procedure.
14 Tottenham Court Road, London, England
(102) 3456 789 / info@joshwilliam.com